|
|
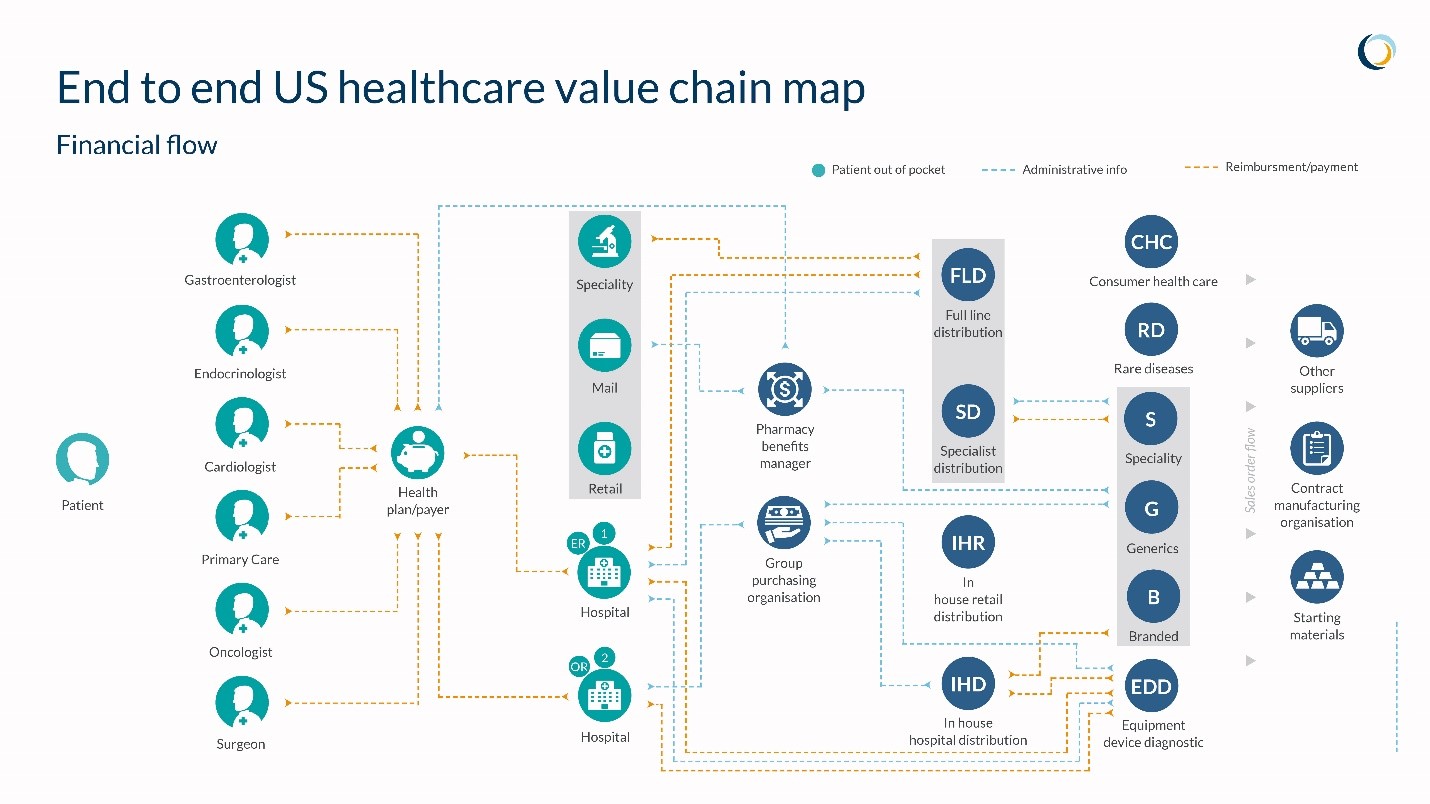
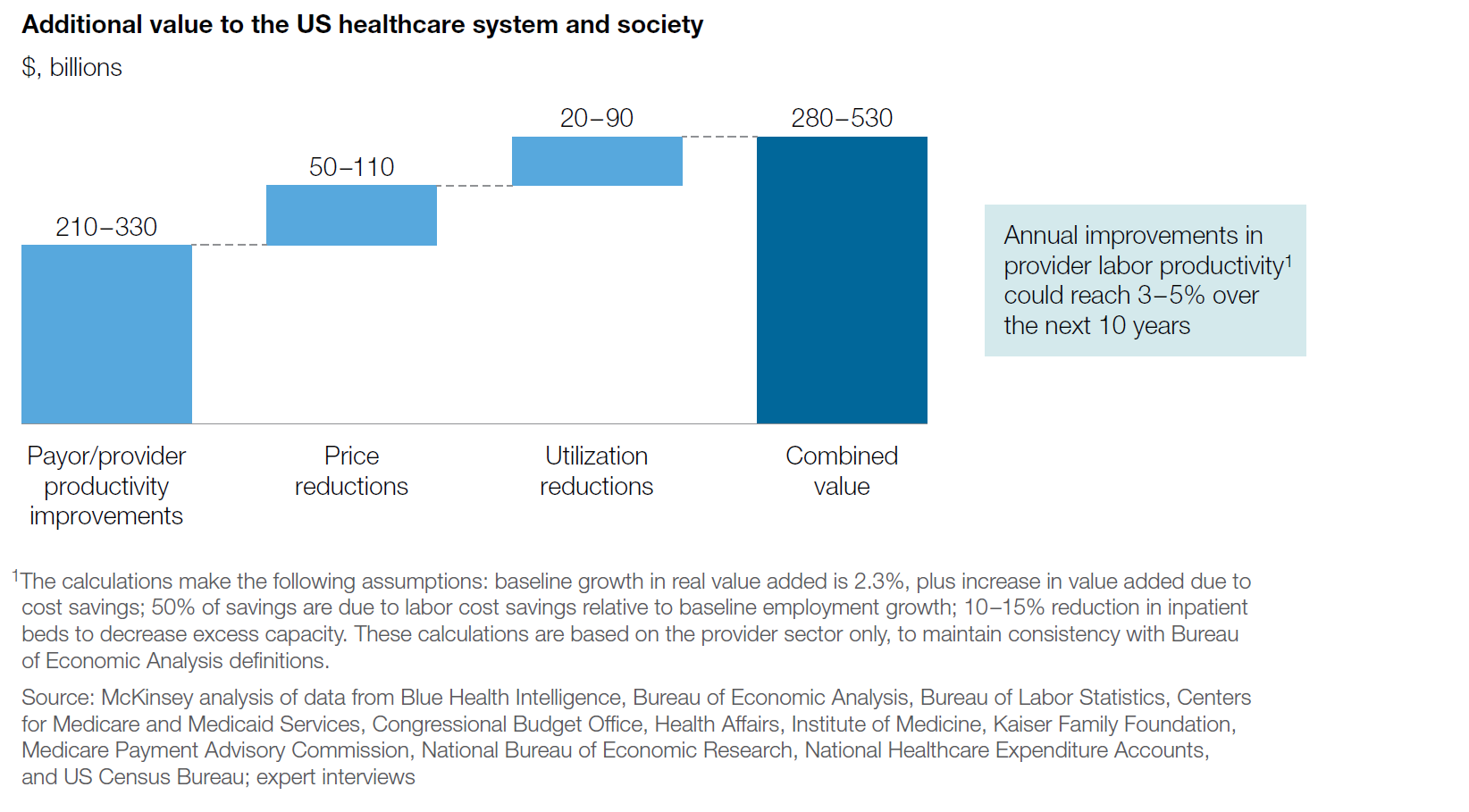
Healthcare's Productivity SinkholeResearch on healthcare productivity typically tells two stories. The first is that the healthcare industry lags far behind other industries in terms of productivity. For instance, US economic data for the years 1995-2005 showed an annual productivity rate of -0.2%. for the healthcare sector. For comparison, the retail industry had a productivity growth rate of 4.3% over the same period (Cutler, 2010). Price changes over time tell a similar story. In 1975 it cost roughly $835 to fly round trip from Chicago to Los Angeles. In 2016, the same trip cost around $217. Compare this to insurance premium changes. In 2005, a family plan averaged $13,000. In 2016, the cost was just over $18,000 (McKinsey 2016). However, some see a different story in healthcare productivity data when factoring in the quality and outcomes of particular treated conditions. One set of researchers saw productivity improvements ranging from .6% to 1.9% for heart attack, heart failure, and pneumonia treatments between 2002-2011. Maybe the situation isn’t as bad as we’ve been led to believe? This is a Story of Healthcare Innovation My guess is that both stories are correct, which gets to the heart of our upcoming Spring Forum on the puzzle of healthcare innovation. Innovation cycles for different aspects of healthcare are wildly out of sync. There are many areas within healthcare where technological or treatment innovations are driving better outcomes and where the money spent on care is significantly lower than the return in quality of life years. However, at the system level, healthcare productivity is like one of those giant sinkholes that open up below housing developments in Florida. Any innovations that positively impact cost or outcomes get swallowed up and lost by the lack of advances occurring elsewhere in the system. People can get hung up the definition of productivity, so to keep it simple, I like this definition of low productivity by David Cutler, a health economist at Harvard: “Less output is produced than is possible with the inputs employed.” Think of the issue of clinician burnout. Would anyone argue that output is greater than inputs? We throw more and more resources into the sinkhole, which only worsens industry productivity. The Solution isn’t Squeezing More Nickels. It’s Overhauling the Financial Model At SCM World, a team of industry supply chain professionals mapped the healthcare value chain from the perspective of a patient with a complex medical profile. We used blinded medical record data from a real patient managing 5 chronic conditions and mapped the physical, informational and financial flow of products and services delivered to this patient. One health system supply chain executive who reviewed the maps admitted that opportunity existed for improvements in the physical flow of goods but felt the greatest opportunity to remove waste was in optimizing the financial flow. Looking at the map below, he said, “we have 2000 people who manage this for us.” Source: SCM World, a Gartner Community I find references to the uniqueness of healthcare unhelpful but it’s hard to deny the impact this administrative/financial model has on the healthcare supply chain professional. In no other industry is payment so detached from the flow of goods and services. Therefore, the supply chain organization finds itself detached from things like customer and patient satisfaction, on time delivery, and product quality since the cash incentive isn’t connected to the delivery of goods and services as it is in other industries. Fixing this may be outside the scope of the supply chain executive, but in my view, it is the signature issue holding healthcare back. Consider the following data from McKinsey on the upside of productivity enhancements in healthcare’s administrative/financial model. Source: McKinsey Price and utilization reductions are important, but these are dwarfed by the opportunity in productivity enhancements across provider and payors. Without tackling the issue of low productivity at this source, the healthcare supply chain professional is going to have no choice but to chase nickels. The profession itself is trapped in healthcare’s productivity sinkhole. I was recently reading Robert Gordon’s book The Rise and Fall of American Growth and while I don’t necessarily believe his premise that the heyday of American prosperity is over, I do believe that we stand a much greater chance of long-term economic vitality if we can radically improve the productivity of the US health system. As always, we welcome your comments and suggestions. |
|
© Strategic Marketplace Initiative | PO Box 1318 | Westborough, MA 01581 | United States | 508 - 732 - 0059 | [email protected] |